Opioid Use Disorder and Treatment: Rural-Urban Comparisons
February 2022
by Per Ostmo, MPA
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration (HRSA), the Rural Health Research Gateway disseminates work of the FORHP-funded Rural Health Research Centers (RHRCs) to diverse audiences. This resource provides a summary of recent research, conducted by the RHRCs, on opioid use disorder.
Prevalence of Opioid Use Disorder in the United States
In 2017, over 70,000 people died from drug overdoses, with 67.8% of these deaths being opioid-related.1 Deaths involving synthetic opioids have increased 71% per year from 2013-2017.1 Fatal opioid-related overdoses resulted in 42,249 deaths in 2016 alone.2 Yet only 35% of those needing treatment for an opioid use disorder (OUD) received treatment from 2015 to 2017.3
Opioid Use Disorder Among Youth and Young Adults
Adolescent substance use is a risk factor for developing OUD or substance use disorder (SUD) as an adult. Between 1999 and 2015, young adults (aged 18-25 years) in nonmetropolitan areas experienced a 411% increase in drug overdose deaths.4 Results from a 2019 survey conducted by the National Institute on Drug Abuse indicate about 6% of youth (aged 12-17 years) have misused prescription pain relievers – nearly all of which were opioids – with no significant difference in use between rural and urban areas for lifetime, past year, and past month misuse.4 However, rural young adults were somewhat more likely than urban young adults to have ever misused pain relievers (15% vs 13%).4
Opioid Use Disorder Among Pregnant Women
Opioid-related hospitalizations for reproductive-age women increased 75% from 2005-2015.5 National Survey on Drug Use and Health data from 2007-2014 indicate nearly 7% of rural pregnant women reported non-medical use of opioids in the past year – more than 19,000 rural women annually.6 Neonatal abstinence syndrome (NAS) and preterm delivery are two significant consequences stemming from maternal OUD.5 According to the Centers for Disease Control and Prevention, newborns with NAS may experience trembling, excessive crying, stunted growth, seizures, and other short- and long-term effects. Lifelong effects of preterm delivery may include cerebral palsy, visual and hearing impairments, and behavioral and social-emotional problems. From 2004-2013, cases of OUD and NAS increased more rapidly in rural counties than in urban counties.5
Treatment for OUD is resource-intensive, and access to these resources may be particularly limited in rural communities.6 Routine screening for substance use for all women of reproductive age may help identify pregnant women affected by non-medical opioid use. Non-punitive policies supporting maternal disclosure of substance use during pregnancy may improve access to medication-assisted therapy.6
Impact of Opioid Use Disorder on Hospitals and Emergency Departments
Higher rates of non-medical use of opioids have increased strain on emergency departments (EDs) with rural EDs facing additional resource constraints compared to urban EDs, such as lower staffing levels, fewer emergency physicians and on-call specialists, fewer training opportunities, and more limited access to advanced medical technology.1
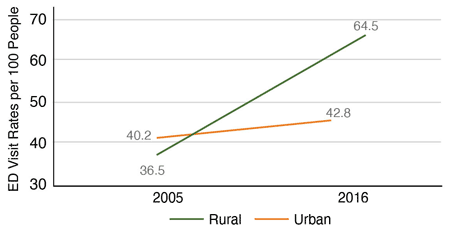
From 2005 to 2016, annual, population-adjusted ED visit rates at rural hospitals rose more than 50%, from 36.5 to 64.5 visits per 100 people, while rates at urban EDs only increased slightly.1 See Figure 1.
Figure 1. Population-Adjusted ED Visit Rates per 100 People1
From 2006 to 2013, rural opioid-related visit (ORV) rates increased 39% (from 64 to 89 per 100,000 visits), while urban rates increased 35% (from 92 to 124 per 100,000 visits).1 See Figure 2.
Figure 2. ORV Rates per 100,000 Visits1
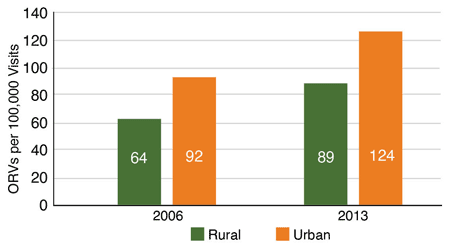
In 2013, approximately 20% of ORVs experienced by rural residents took place in urban EDs. In comparison, only 15% of non-ORVs experienced by rural residents took place in urban EDs.1 Possible explanations for this difference include avoiding rural EDs to escape local stigma, decisions made by first responders to divert severe illness directly to urban EDs, and limited trauma or intensive care services available in rural EDs.
In 2015-16, rural older adults (aged 65 years or older) were more frequently prescribed opioids than their urban counterparts. Additionally, a greater proportion of ORVs in rural EDs than urban EDs consisted of older adults. However, it is unknown if these older adults were experiencing OUDs, or if they were taking opioids as generally prescribed but experienced an overdose because of confusion about appropriate dosing.1
Prescribing Buprenorphine for Opioid Use Disorder
Drug Enforcement Administration (DEA) waivered physicians may prescribe buprenorphine for the treatment of OUD, but many waivered physicians are not utilizing waivers to their full extent, which contributes to the lack of OUD treatment access.2 In a 2016 survey, DEA waivered providers reported time constraints, reimbursement concerns, practice partners’ resistance, attraction of drug users to their practice, and DEA intrusion as barriers to incorporating this service into their practices.2 Few physicians with either the 30- or 100-patient waivers were at or approaching their limit. Approximately 89% of waivered physicians reported having prescribed buprenorphine for OUD, with only 56% currently accepting new patients for treatment. Physicians with a 30-patient waiver were treating, on average, 8.8 patients, but 53% were not treating any patients. Those with a 100-patient waiver were treating, on average, 56.9 patients.7
Partial Psychiatric Hospitalization Programs
Partial psychiatric hospitalization programs (PPHPs) are intended to reduce or avoid inpatient psychiatric stays by allowing persons to reside at home while receiving structured care. Arranging psychosocial and post-emergency care for patients is challenging because rural hospitals tend to have limited resources. For comparison, 38.7% of metropolitan hospitals versus 11.4% of nonmetropolitan hospitals offer any PPHPs.8 Financial or other policies that encourage rural hospitals to expand PPHPs could increase access to SUD/OUD treatment.8
Resources
- Maine Rural Health Research Center (2021). Opioid-Related Visits to Rural Emergency Departments.
- WWAMI Rural Health Research Center (2018). Overcoming Barriers to Prescribing Buprenorphine for the Treatment of Opioid Use Disorder: Recommendations from Rural Physicians.
- Rural and Underserved Health Research Center (2020). Early-Career and Graduating Physicians More Likely to Prescribe Buprenorphine.
- Maine Rural Health Research Center (2020). Substance Use Among Rural and Urban Youth and Youth Adults.
- University of Minnesota Rural Health Research Center (2018). Practical Implications: Opioid-Affected Births to Rural Residents.
- University of Minnesota Rural Health Research Center (2018). Non-Medical Opioid Use Among Rural and Urban Pregnant Women, 2007-2014.
- WWAMI Rural Health Research Center (2018). Prescribing Practices of Rural Physicians Waivered to Prescribe Buprenorphine.
- Rural and Underserved Health Research Center (2019). Partial Psychiatric Hospitalization Program Availability in Nonmetropolitan and Metropolitan Hospitals Nationally.
