Rural Hospital Closures
December 2017
by Shawnda Schroeder, PhD
Funded by the Federal Office of Rural Health Policy (FORHP), under the Health Resources and Services Administration, the Rural Health Research Gateway strives to disseminate the work of the FORHP-funded Rural Health Research Centers (RHRCs) with diverse audiences. The RHRCs are committed to providing timely, quality national research on the most pressing rural health issues. This resource is one of two providing a summary of their most recent research on hospital closures.
Rural and urban hospitals serve varied patient demographics. Urban hospitals are located in counties with 20% higher income than rural hospitals, and isolated rural hospitals provide care in counties where one-fifth of the population is elderly.1 As a result of patient demographics, reimbursement models, market characteristics, and available services (among other variables), rural hospitals are closing and rural communities are losing services in higher proportion than urban communities. The financial distress index (FDI) was developed to identify rural hospitals' risk of financial distress and has been a useful tool in identifying at-risk hospitals, providing an opportunity for rural hospitals and communities to consider alternative service models. This research also opens the door to future study of policy options and the communities impacted by hospital closures.
Hospitals in the United States
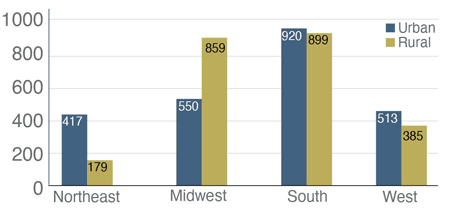
In 2012-13, the U.S. had about 5,000 short-term, acute care hospitals; half were located in urban areas, and half were in rural areas.1 Among rural hospitals, 39% were located in large rural areas, 39% in small rural areas, and 22% in isolated rural areas.1 The largest number of hospitals were located in the South.1 See Figure 1.
Figure 1. Number of Hospitals by U.S. Census Region and Rural/Urban Status (2012-13)1
Hospital Closures
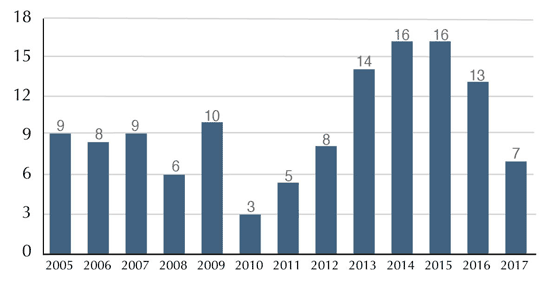
From January 2005 to November 8, 2017, 124 rural hospitals closed in the U.S.2 See Figure 2. The most current number of rural hospital closures can be found at The Cecil G. Sheps Center for Health Services Research. Predictors of rural hospital closure have included financial distress,2 hospital size, and community poverty rates.3
Figure 2. Number of Rural U.S. Hospital Closures, January 2005 through November 20172,4
As a result of hospital and obstetric-unit closures, there was an increase in the percentage of U.S. rural counties without any hospital obstetric services from 2004 through 2014 (from 45% to 54%).5 During this period of time, 179 rural counties experienced closures/loss of hospital obstetric services.5 In 2014, while 77.9% of micropolitan (urban) counties reported access to hospital obstetric services, only 30.2% of rural noncore counties had access.5
Financial Distress Index
An FDI was developed to determine if a rural hospital could be classified at a high, medium-high, medium-low, or low risk of financial distress.3 The FDI model “includes 12 predictors composed of 4 measures of financial performance, 2 measures of hospital characteristics, 2 measures of government reimbursement, 2 measures of community characteristics, and 2 measures of local competition.”3 Access the brief Prediction of Financial Distress Among Rural Hospitals for a complete list of factors utilized to determine risk.3
Between 2006 and 2014, hospitals identified as high risk in the FDI had closure rates 60 times higher than hospitals identified as low risk.
- Two out of three hospitals that closed were identified by the FDI at high risk of financial distress in the year prior to closure.3
- The proportion of rural hospitals at high risk increased from 7.0% in 2015 to 8.1% in 2016.3
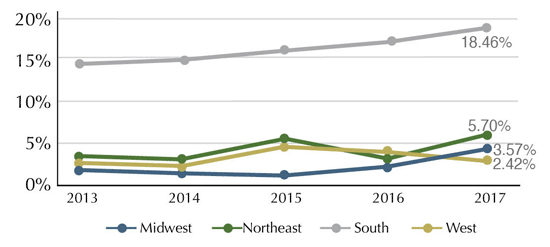
- The South Census region reported the largest percentage of hospitals at risk in 2017.2
States with the highest number of rural hospitals at high risk of financial distress in 2015 were Texas, Oklahoma, Tennessee, Arkansas, Georgia, and Alabama.6 States with the highest percentage of rural hospitals at high risk included Hawaii, Alabama, Oklahoma, Arkansas, and Tennessee.6 The South Census region reported a greater percentage of rural hospitals at high risk of financial distress than any other Census region.6 See Figure 3.
Figure 3. Percent of Rural Hospitals at High Risk of Financial Distress, Census Region, 2013-20176
Urban and Rural Hospital Profitability
Insufficient revenue reduces hospital services and quality, which can lead to closure.7 Hospital closures leave rural residents at greater risk of health and economic hardships because of the loss of local acute and inpatient care services.7 Medicare Dependent Hospitals (MDHs) reported a larger percentage of their hospitals at high risk of financial distress than any other rural hospital type in 2016.6 However, the percentage of rural Perspective Payment System (PPS) hospitals and Rural Referral Centers (RRCs) at high risk consistently increased from 2013 through 2016.6 See Figure 4.
Figure 4. High Risk of Financial Distress in Rural Hospitals, by CMS Payment Type, 2013-20166
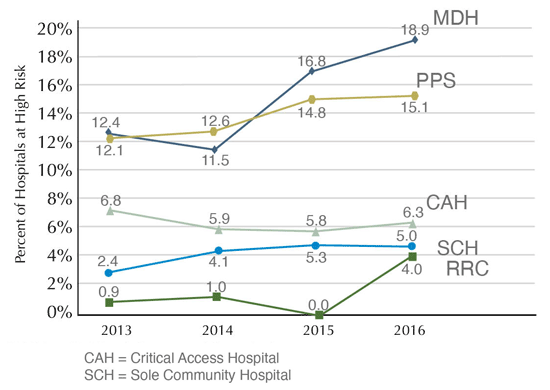
RRCs and urban hospitals had higher profitability when compared to other hospitals.7 The rural PPS hospitals (26-50 beds) and MDHs had lower profitability with high financial distress when compared to other payment systems.7 From 2012 through 2014, urban hospitals experienced increases in profitability while rural hospitals experienced decreases.7 The Rural Health Information Hub's Rural Hospital topic guide provides basic information on these hospital types.
Resources
- North Carolina Rural Health Research and Policy Analysis Center (2015). The 21st Century Rural Hospital: A Chartbook.
- North Carolina Rural Health Research and Policy Analysis Center (2016). Trends in Risk of Financial Distress Among Rural Hospitals.
- North Carolina Rural Health Research and Policy Analysis Center (2016). Prediction of Financial Distress Among Rural Hospitals.
- North Carolina Rural Health Research and Policy Analysis Center (November, 2017). Rural Hospital Closure Tracking Website.
- University of Minnesota Rural Health Research Center (2017). Closure of Hospital Obstetric Services Disproportionately Affects Less-Populated Counties.
- North Carolina Rural Health Research and Policy Analysis Center (2016). Geographic Variation in Risk of Financial Distress Among Rural Hospitals.
- North Carolina Rural Health Research and Policy Analysis Center (2016). Geographic Variation in the Profitability of Urban and Rural Hospitals.
